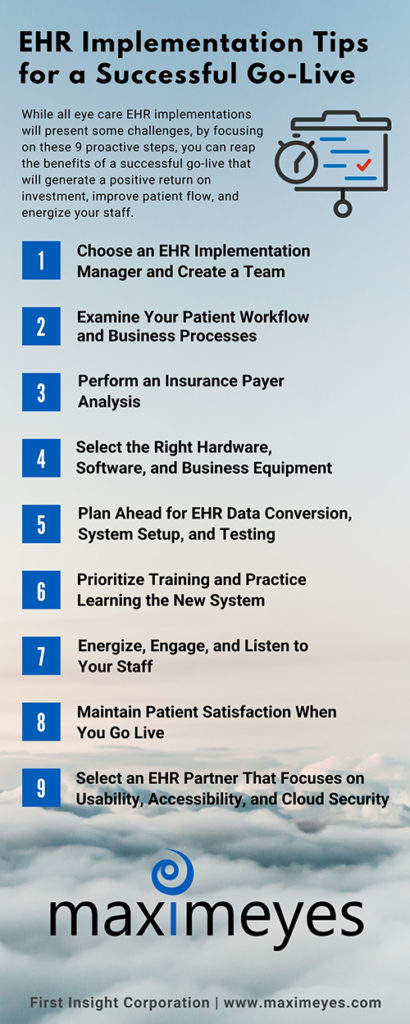
26 Oct 9 EHR Implementation Tips for a Successful Go-Live
EHR implementation for your eye care practice is a process (strategies and steps) that takes time, patience, and commitment to reach a successful outcome.
Poor planning, poor communication, and insufficient training will lead to undesirable results if you set unrealistic expectations and close communications with your staff.
Choosing a new cloud EHR partner is one of the most significant business decisions you’ll make for your eye care practice. Technology is a huge investment, and you need to know that investment is worth it.
The average optometry EHR implementation takes around eight weeks to complete, although this can vary based on the practice (size, location, providers). It’s critical to set aside time for system setup, training, and quality reviews to keep your Go-Live on track.
While all EHR implementations will present some challenges, by focusing on proactive steps, you can reap the benefits of a successful Go-Live that will generate a positive return on investment, improve patient flow, and energize your staff. Here are a few proven EHR implementation steps to help guide you along the way.
1. Choose an EHR Implementation Manager and Create a Team
An EHR implementation manager should have the skills, training, and time to form, lead, and facilitate a team. While MaximEyes assigns you a dedicated implementation coordinator during your EHR onboarding, appointing an implementation manager within your practice will ensure consistent communication and a smooth transition.
Form a highly-skilled EHR implementation team and designate super-users from your practice who will embrace change, contribute enthusiastically, and have the respect of their peers.
Implementing an EHR system should not be driven solely by IT. Implementation requires the involvement and commitment from every practice level. Develop and follow a plan so your team can track EHR and practice management implementation challenges, issues, decisions, and assigned tasks.
Pro Tip: Use Google Workspace™ (formerly Google G Suite™) to collaborate on files in real-time. Google Workspace comes with security built-in, so your data, devices, and files are protected and backed up in the cloud. Google Workspace supports HIPAA compliance; however, you have to sign a Business Associate Agreement (BAA) with Google Workspace for Protected Health Information (PHI) compliance.
2. Examine Your Patient Workflow and Business Processes
Once you analyze every function of every job, you can understand how your staff accomplished those tasks with your old EHR and practice management system. Create an assessment of the level of proficiency for each employee’s level of performance.
Now it’s time to build a comprehensive, clear roadmap of your patient workflows and office processes that include the following:
- office infrastructure modifications
- hardware installations
- software configurations
- ophthalmic equipment and image management system integrations
- backup systems
- entering old patient data in the new EHR system
- cloud performance and security
3. Perform an Insurance Payer Analysis Before an EHR Implementation
Moving to a new optometry practice management system may require new Electronic Data Interchange (EDI) agreement enrollments (differs from payer to payer) so you can continue to submit electronic claims.
If you outsource your eye care billing to a third-party company, notify them weeks in advance that you will be moving to a new practice management system to prevent serious revenue problems or denied/rejected claims.
Are you searching for an efficient end-to-end revenue cycle management partner? Fast Pay Health’s certified coders and optometric billing consultants have extensive experience in optometry and ophthalmology coding. Coders are well-versed in CPT® and ICD-10 coding, eligibility and benefits verification, provider credentialing, billing with code modifiers, EDI processes, industry standards, and maintaining 100% HIPAA compliance.
4. Select the Right Hardware, Software, and Business Equipment
To ensure optimum software performance and data integrity, use high-quality hardware, and exceed minimum hardware requirements to stay ahead of advancing technology. Focus on your future needs, not just immediate needs, because they will change.
Always refer to your EHR vendor’s hardware and software system requirements. Only use the equipment and operating systems that your EHR vendor supports and tests. Ask your EHR vendor if your ophthalmic diagnostic equipment is compatible with the new EHR system and if it can transfer readings to the patient’s electronic health record.
Discuss other ophthalmic and business equipment with your EHR partner before purchasing new equipment, such as high-output laser and label printers, barcode, insurance card, and document scanners.
Pro Tip: Perform ongoing (at least bi-annual) hardware audits (workstations, laptops, tablets, routers, modems) to ensure your equipment is compliant and is keeping up with the latest requirements. Audits help you identify if the equipment is outdated and reveals potential compliance and security vulnerability issues.

5. Plan Ahead for EHR Implementation Data Conversion, System Setup, and Testing
One of the first steps your eye care EHR partner will ask is for you to complete an EHR implementation questionnaire and onboarding sheet. Don’t delay with completing this critical step. Once you define the migration parameters, your practice will provide a system backup to the EHR onboarding team to begin setup and testing the final data conversion.
Whether you are converting paper records to electronic records or transitioning from one EHR to another, allow plenty of time for migrating and testing your data in your new EHR system. Confirm with your EHR partner that they can migrate and map legacy data (if available and accessible) to new database fields from your existing system.
6. Prioritize Training and Practice Learning the New EHR System
The best way to learn a new ophthalmology or optometry EHR system is to practice. Use the system from check-in to check-out based on your existing workflows, noting any questions you have along the way. Insufficient training can lead to unsatisfied employees, high turnover rates, mistakes, and lost revenue.
Take notes on any questions you may have when using the practice management and EHR software and review all training materials. Share the notes with your EHR implementation coordinator during your training sessions.
Give yourself and your staff dedicated (uninterrupted) time to review training documentation and practice using the software. Reduce learning overload. If you try to do too much too quickly, you and your staff will get frustrated and give up while juggling a full patient schedule.
Don’t rush the EHR learning process—you don’t need to know how to use every feature in the system. Ensure staff knows where to get answers to questions, whether through training guides, an office “super-user,” or your EHR customer support.
Take advantage of your EHR online training resources. MaximEyes.com’s self-guided Integrated Learning Center streamlines your training experience. The Learning Center is built-in to MaximEyes.com and is accessible 24/7. Download documentation, view video overviews, engage with step-by-step walkthroughs, and complete courses without ever leaving your software.
7. Energize, Engage, and Listen to Your Staff
As with any new process, moving to a new EHR system often requires a change in employee attitudes and behaviors. Even though your staff may agree with the concept, several may have a low tolerance for change.
Energize and engage employees and reinforce that you can’t do this alone. Offer incentives to employees and address “what’s in it for them.” If you commit to a successful EHR rollout, your staff will move forward with a more positive approach.
Ongoing communication is essential. During implementation, you may need to meet daily or weekly with your staff. After implementation, schedule monthly meetings. Brainstorm and allow your team to be honest about their concerns and recommendations. People want to be heard. Agree to disagree as healthy disagreements lead to better outcomes.
8. Maintain Patient Satisfaction When You Go Live
Patient flow management impacts staff performance, patient experiences, and revenue growth. When a patient enters your practice, each point of contact is an opportunity to build trust and gain patient loyalty.
Avoid a long delay between training sessions and the EHR implementation Go-Live date. Close your office the first day you install your new EHR software, and reduce your patient load the following day. Book appointments lightly during your initial training so doctors and staff can focus on a “hands-on” approach.
9. Select an EHR Partner That Focuses on Usability, Accessibility, and Cloud Security
Now that you know the critical areas you should focus on before, during, and after your EHR implementation, you can start collecting information about your top EHR software choices to run a successful eye care practice.
Look for a practice management and certified EHR system that focuses on your future goals, not immediate needs. So you can spend more time supporting your patients and expanding your eye care business, your EHR partner should align with your long-term vision.
MaximEyes.com, First Insight’s newly rewritten, redesigned, and unified eye care cloud-based certified EHR and practice management system for optometry and ophthalmology is optimized so you can access data—anywhere, anytime, from any device—from your web browser, or via a local server, if that is your preference. Rest assured that we monitor and adhere to secure cloud EHR data protection, backup, and disaster recovery.